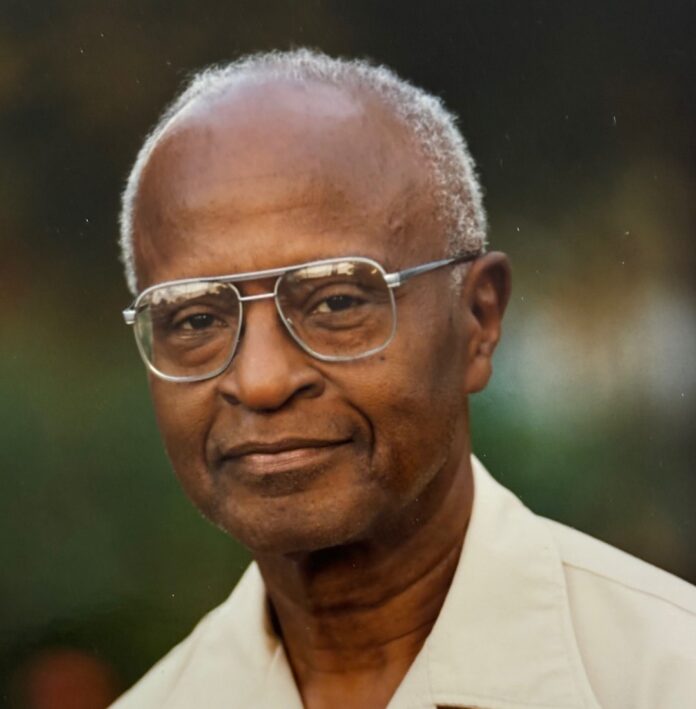
Dr. Sydney Fitz Barnwell, born in British Guiana, now Guyana, in September 1926, passed away on March 29, 2024, at the age of 97.
Dr. Barnwell’s migrated to the USA in 1947 and his academic journey commenced with distinction as he graduated with honors from Howard University with an undergraduate degree after three years, followed by his graduation from Howard Medical School in 1955. He then completed an internship at D.C. General Hospital in Dermatology Pathology before briefly returning to Guyana and subsequently resuming his medical career in the United States.
His professional pursuits led him to internships at Providence Hospital in Baltimore and Mercy Douglas Hospital in Philadelphia from 1960 to 1963. Achieving board certification in 1963-64, Dr. Barnwell later served as a surgeon at the VA Hospital in Tuskegee, Alabama, caring for many Black veterans.
In 1965, Dr. Barnwell settled in New Bern, North Carolina, where he made history as the first African American surgeon in Eastern North Carolina. He dedicated two decades to serving at Good Shepherd Hospital, a segregated institution for Blacks, where he performed a wide range of surgeries, including tonsillectomies, hysterectomies, bone surgeries, and general abdominal procedures. His commitment extended to Craven County Hospital, where he held surgery privileges, although most patients were transported to Good Shepherd Hospital for postoperative care.
Dr. Barnwell’s contributions extended beyond surgery. As Medical Director of the Craven County Health Department, he implemented a groundbreaking prostate cancer prevention and detection program, significantly reducing mortality rates among African American men in Craven, Jones, and Pamlico Counties.
After relocating to Tennessee in 1985 to work at Meharry Medical College and the VA Hospital, Dr. Barnwell returned to New Bern in 1998 as the Medical Director of the Health Department until his retirement in 2015.
Despite retiring, Dr. Barnwell remained actively engaged in community affairs and received numerous accolades, including the NC Citizen of the Year Award in 1984 and the Order of the Long Leaf Pine in 2002. His dedication to public health and social justice, coupled with his mentorship and wisdom, enriched the lives of many.
Dr. Sydney Fitz Barnwell is survived by his daughter, Maria Barnwell, son, John Barnwell, and three grandchildren, Ava Lehner, Dylan Lehner, and Xavier Barnwell. His legacy as a healer, advocate, and community leader will endure for generations to come.
Guyana Graphic extends our deepest condolences to Dr. Sydney Fitz Barnwell and his family in New Bern, North Carolina. During this time of loss, our hearts are with you, and we share in your sorrow. Dr. Barnwell’s contributions, both professionally and personally, have undoubtedly left a lasting impact. May cherished memories bring solace, and may you find strength in the love and support surrounding you. Our thoughts are with you during this difficult time.
Oral History Interview with Dr. Sydney Fitz C. Barnwell
Collection Number: Date: May 21, 2001 Narrator: Sydney Barnwell, MD Interviewer: Ruth Moskop, PhD, and Paul Cunningham, MD Transcriber: Janipat Worthington
Copyright 2001 by East Carolina University. All rights reserved. No part of this document may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from East Carolina University.
RM: I am Ruth Walker Moskop. I am here at the Surgery Library at the Brody School of Medicine in Greenville, North Carolina. Today is May 21, 2001, and I am here to do a preliminary interview with Dr. Sidney Barnwell who has come to visit from New Bern, North Carolina. Dr. Barnwell, good morning.
SB: Good morning.
RM: It’s so nice to have you with us.
SB: Good to be here.
RM: Do we have your permission to record this interview?
SB: Yes, you do.
RM: Well, I’m so glad. It’s a privilege to be a part of this process. The question I would like to ask you is-you told me that you came to eastern North Carolina in 1965-and I am wondering if you could compare the situation then. I understand you were a surgeon at that time as well? you came here as a surgeon, and how were things in those days-in the 60s? Well-a little more background-between the ’60s and ’70s, there was a 10-year struggle to found a medical school here at East Carolina University. Were you aware of that struggle?
SB: Yes, very much so. I came in ’65. In fact, I was invited to go to New Bern in 1965 because there was a black hospital there without a doctor, and this was the Good Shepherd Hospital? about a 65-bed hospital. I left Tuskegee VA Hospital around July of 1965 and ended up in New Bern. I intended to stay for a year because I wanted to go back to Guyana to practice surgery, but things didn’t work out well in Guyana so I stayed in New Bern. Around 1965, there were various, different dynamics. The civil rights dynamic was working. I knew that there was an effort in the late ’60s/early ’70s to establish a medical school here because I was very active in the Old Northstate State Medical Society, and of course Dr. Best kept me abreast of what went on here. I am quite aware of the enabling legislation that got the medical school. The Old Northstate State Medical Society played a great part in getting this medical school started-the votes in the Legislature, etc. I was aware of that. I was aware also of the civil rights tensions in the 1960s. When I got to New Bern, the situation was very segregated in 1965. The hospital there-the Good Shepherd Hospital-was founded in approximately 1932. In the 1920s, there was a great fire in New Bern, and black folks felt that they were not given good treatment after the fire-those who were injured. So, many churches came together, and one church in particular-The Episcopal Church-headed the drive to get a black hospital in New Bern, and so the hospital flourished, did well in the ’40s and ’50s, and for some reason, the other doctors who were there went for additional training, and in perhaps 1963-1964, there was no doctor. Many doctors who practiced in the Craven County Hospital at that time-and the Craven County Hospital was somewhat new also–those doctors came over to the segregated hospital-the Good Shepherd Hospital-but the administrator felt they needed a doctor who would give somewhat full-time treatment to that hospital. So, I left Tuskegee VA Hospital, came up, and sort of fell in love with New Bern after the first year. Besides the practice of surgery, I did a lot of general practice. At one time, I had 33 patients-myself and that hospital. It actually opened two years after I got there, and there was full integration in 1968 or so with the Craven County Hospital, and I went over to the Craven County Hospital. I should tell you also that I had full privileges at Craven County Hospital even though I spent most of my time at the old Good Shepherd Hospital.
RM: What happened to the Good Shepherd then when Craven County integrated?
SB: Well, it is now still a building, but it’s a nursing home.
RM: Isee.
SB: Yeah, a nursing home. Most blacks of course, after it closed, went over to the larger, more equipped hospital, which was the Craven County Hospital at that time.
RM: Well, when Dr. Best started talking to you and the others in the Old Northstate Medical Society about the need for a medical school at ECU, how did you react to that? Did you agree with him spontaneously-yes, we need a new school; we need better medical facilities-or how did you react? Did you think the situation was under control healthcare-wise?
SB: Well, I was aware of what we called an eastern phenomenon. In Virginia, there was one. In Tennessee [there] was one. In North Carolina, I guess they were just coincidental, but in our area, you know, we were just agricultural, and most people had to go to Duke or Chapel Hill for their tertiary care, and we felt that we had the population and we had the need for a medical school here. The emphasis also was placed on family practice because in the ’60s and ’70s and perhaps in the ’80s, people were just thinking of tertiary care without a fundamental kind of care that you get from the family practitioner. I am glad the Old Northstate and those who conceived the idea thought that this medical school should emphasize training family practitioners; and that came about, and we were well behind it. The need was there. The idea of the assessment of the whole area, 21 or so counties, I think there are more than 21 counties in this area-the eastern portion. I was thinking politically [of] all21 counties that we thought of in politics. We needed the basic care-family practitioner care-and of course with that as an initiation of this medical school, specialties grew out of that.
RM: Can you help us understand, those of us who were not here, those of us didn’t practice healthcare in eastern North Carolina, primary care medicine and surgery as you did both-can you tell us some stories that would help us visualize how it was if you were the sole, black healthcare provider in Craven County? Well, that’s not true-the licensed physician.
SB: Well, I was when I got there-the sole black practitioner in Craven County.
RM: I can imagine that patients came to you with all sorts of problems that may have been avoided had they had intervention.
SB: Well, it was just hard work. I mean, you had to be prepared to be called out at 2:00 in the morning and then proceed with what you had to do at 8:00 the next morning. At that time, being a sole practitioner was something which was accepted. In the larger, white community of doctors, we had a few doctors who got together in groups. When I came in 1965, there were three certified general surgeons-white general surgeons-in Craven County, and I was certified prior to coming to Craven County. There was the usual competition for patients, perhaps early on, but that wasn’t seen very much because I filled a void. Many of those people I treated couldn’t afford to pay the doctor, and insurance wasn’t something that most people had.
RM: Sure.
SB: So, I was able to fill that void-those non-paying people who needed medical care. And I think that is part of practicing Medicine-you go into Medicine not because people have money but because they have a need for care. And so, I just did that. But the other part of it, the people received you so warmly. You are the doctor. Dr. Barnwell, you know. And wherever you went, you felt that you were welcomed in the black community and needed and performed a useful service. The problem came in those days-the white community, how can you overcome that by… One thing I had in my favor, I was board certified. I was the only board-certified surgeon in eastern North Carolina, so that worked very well for me.
RM: I should say.
SB: The other thing is-it was easier for me to work with white physicians. I didn’t have that historical baggage because I came from another country, so it was easier for me to do that. But later I ran into some problems. After the first two or three or four years, another surgeon came into the area-Dr. Charlie Ashford. He was Johns Hopkins-trained, and he came with his chest boards. You know, he was certified in chest surgery. He and I were able to work together, where the other three surgeons were in partnership. One of those three was Simmons Patterson who went on to be very prominent in the state in cancer. And then those three multiplied to four, but Dr. Charlie Ashford and I worked very closely together. [He came] around 1969-1970. He and I were somewhat close. I would help him, and he would help me. As a general surgeon in those days, you had to do most things-tonsils, hysterectomies, pin fractures, the general surgery, abdominal work, so I sometimes think I was one of the last of the really true general surgeons.
RM: Yeah.
SB: Yeah. When Ashford came, he brought to my attention the vascular surgery, so he and I were able to get into that.
RM: Were you able to seek healthcare elsewhere for patients who needed the tertiary care that you said was not available?
SB: The tertiary care was available, but you had to get in touch with Duke or Chapel Hill. That made it very… because the patient gets lost, and you don’t know what transpired. Then the patient appears back to you. There wasn’t that nice, easy transition.
RM: Can you describe what kinds of cases you would have to send to Chapel Hill and Duke?
SB: Well, neurosurgical cases. That’s one. Difficult vascular work cases. We were probably… In 1965-1966, around 1967, a board-certified orthopedic surgeon came to New Bern. Then, I gave up most of that work. But prior to that, difficult orthopedic cases were sent to Duke.
RM: What about chronic illnesses-sickle cell anemia or…
SB: Well, that type of case, you know, I didn’t deal with it because primarily I did surgery. If a patient came into my office with sickle cell anemia, I would seek help because that is something right now I don’t know how to handle very well.
RM: And where would you go for support with that?
SB: Well, the support would come from the internist in our area. If he or she was not able to handle that, we would send the patient over to Duke or Chapel Hill for that type of thing. I enjoyed doing surgery for the few years, well actually more than few years, from ’65 to ’85. For the first 10 years, it was very enjoyable practicing-very hard work. But as I said, I got that support from Ashford. It got a little difficult after the first 15 years. More doctors came into the area-more complications-and I found that it was the first time I ran into what I thought was prejudicial kinds of behavior in some doctors; this was approximately 1982.
RM: After more physicians had come into the area.
SB: Yeah, and I began to see what most black doctors were telling me about. Hey, these guys are not right. Something is wrong, you know. But something else kept me in this area. It was the presence of the medical school. And that’s an interesting story. Before I get to that, remind me… Let me tell you another interesting story. About 1967, I was in my office and in came the medical director of the Health Department and his nurse. I think it was Dr. Brown and Mrs. Sykes. After seeing a few patients, Dr. Brown came to the office and said, ‘I would like you to work at the Health Department.’ I was curious because he knew I was a surgeon and he wanted me to work at the Health Department. Of course, I said, ‘Look, doctor, you know, I did all this training in surgery, and I know very little about prenatal care and maternity care…’
RM: Infectious diseases…
SB: And of course, he tells me most of his problems, but after about 15-20 minutes, I said, ‘I can’t help you.’ Then, he did something which I’ll never forget. I sometimes see it in the movies, you know. Bette Davis and the old actresses-in order to make the point-they get up, go to the door, and before they can get out of the door, they turn around and make a point. This is what Dr. Brown did: He got up, went to the door, and turned around. He said, ‘Dr. Barnwell, they’re all black. They’re all black.’
RM: All the patients at the Health Department?
SB: Yeah-that he wanted me to see. Well, I was caught. I went down to the Health Department and did prenatal work, maternity work… I did what he wanted me to do for three or four years. Once a week I would go down and do these things. The nurses were well prepared, and that’s how I got hooked up with the Health Department. Another incident around 1970-family planning was introduced and, of course, the Health Department didn’t want to touch that-that came down from the federal government. So they had family planning-we’re talking about the pill then-and somebody came to my office with the same line: ‘Dr. Barnwell, we’ve got all these girls who are going to get pregnant and so, so, so, so, so. Are you going to help us?’ And so I went then. Once a week-family planning. You know, in those days we had the IUDs and lots of pills, etc. So I got into family planning until 1985. Family planning got absorbed in the Health Department and, again, after dropping the prenatal and the maternity [work], I stuck with family planning until1985. Once a week, I would go to the Health Department to do the difficult things that the nurses couldn’t do. So that’s how I got hooked up in the Health Department. Now, another thing I wanted to tell you-a most interesting story. During my surgery training, I did a lot of pathology-a complete year of formal pathology as a resident-and I loved surgical pathology because I felt you had to know that to be a good surgeon. Around 1969-70, the medical school had started, didn’t it?
RM: A one-year school. That’s right.
SB: Around 1970?
RM: Uh-huh.
SB: So around 1970-1971, I came over to the Pathology Department-Or. Beekman-and told him I was interested. I wanted to keep up with some of the surgical pathology, and he said, ‘Okay, what can we do?’ But he had a problem, and I didn’t know what his problem was until he told me. The problem here was the hospital was-let me use a word because I don’t know the right word–commandeered-by the medical school. The hospital that’s here was here before the medical school.
RM: Right.
SB: It was the County Hospital. So the medical school came sort of superimposed, and Dr. Beekman was assigned as the chief pathologist. But there were some other pathologists here who were entrenched, and for some reason or the other, the school could not use all the facilities of the Pathology Department to train medical students. That was just one of the early problems they had, and I came to Beekman at the same time. So I proposed to Dr. Beekman, ‘Look. Let your students come to Craven County Hospital, and I will do what is necessary over there to help in the training of …’
RM: Their pathology training…
SB: Yes. So once a week, students came-a busload of them came over-and, you know, we saved specimens. The hospital was receptive, and we did that for a year to two years. So I got with Dr. Beekman, and that was a successful program. Students loved to come down, and I really prepared myself when they came, and they brought back a lot of specimens, which I suspect was hard to get at the hospital here. So that worked well. Two or three years after that, I was made Associate Professor of Surgical Pathology. Yeah, it was impressive. And then approximately 1975, Dr. Laupus, the dean, came to see me in my office. He wanted me to be Assistant Dean for Minority Affairs at the medical school, and so I came up here for about four years to the medical school to fulfill that role-Assistant Dean for Minority Students or something like that. Of course, I also came once every two weeks or so to the Surgery Department, and Dr. Pories was here. They had big conferences, and that helped me with my academics and sharpened my thinking-coming to these conferences. So I had a close association with the medical school and a close association with the Health Department. My financial man told me just before I left in 1985, he said, ‘Look, you gotta do more surgery and risk some of the other things.’ But by that time, I was ready to leave. Another offer came in 1984-85, and I left and went to Meharry Medical College in Nashville, Tennessee.
RM: And you stayed on the faculty there?
SB: Yes, and that was a different experience-that was a different experience. Working in Tennessee is a different world, different dynamics. Meharry Medical College is about 130 years old. Vanderbilt is the dominant medical school in the area, and Meharry financially was always in distress. Vanderbilt was well endowed, and there was competition for resources. Around 1985, Meharry was able to get into the general hospital to train some medical students. Vanderbilt enjoyed that for years-the general hospital. So I went to head up the Surgery Department at that general hospital for Meharry, so I had to work very closely with Vanderbilt, and that was a different experience.
RM: Different experience, yeah. There are other stories that people have shared with us about that situation-the tension between Meharry and Vanderbilt. It’s really heartbreaking in many cases.
SB: Well, again, the challenges, you know … As I said, when I came here, the black-white thing was obvious. The challenge was trying to overcome whatever barrier. And, as I said, the first 10 years, 15, it was fairly easy for me to get through that. One of the assets I brought-! wasn’t born in this country.
RM: What changed socially and administratively? I mean, from the government, we legislated integration, but yet that seemed to somehow make it worse for you. You said you were able to get through it for the first 15 years but then something happened, and it…
SB: Well, I didn’t know competition. Lots of doctors came to New Bern. When I got to New Bern, there were about 35 doctors, and by the ’80s, there were 85-1suspect there were about 100 doctors in the area, and there were different tensions. There was a tension building up between Craven County Hospital, which is now called Regional Authority or something, and the medical school, the Surgery Department… While perhaps those in Greenville were not aware of it, surgeons were very keen of the competition also because many of their patients went to Greenville.
RM: Down to Greenville then-a newer facility, I guess.
SB: It was a newer facility. Then younger surgeons came, and they felt they were as well trained as any surgeon over here, and so that competition was… Those tensions… And I was associated with this medical school. ‘Why are you associated with this medical school? Why don’t you stick with us and build some autonomy in Craven County?’ So, those tensions came about? different dynamics. The life expectancy of a black man in this country is 65. If you add 10 years to that right now, you get a life expectancy of a black woman and a white man-75. Add 15 to that to get 80-the life expectancy of a white woman. And if you focus on that black man right now at 65, his life expectancy is lower than the life expectancy of a black man in Jamaica, in Barbados, and Cuba of all places. And we all got off the boat at the same time. You know, about 5% of the slaves from West Africa came to the United States. Ninety percent went to Brazil and the West Indies. The genetics are about the same, so there are some dynamics in this country… Where it started, I don’t know-early in the century-that blacks have actually less exercise and more of the undesirable food intake, and we can see it right now. I don’t know how to tum this thing back around; that’s one of my new efforts now, to try to reverse this.
RM: I’m assuming that white men eat just as many sausages and pancakes as black men do, though, and so why is their life expectancy longer?
SB: All right. If you are in a white community, any white community in this country, you see other white folks walking and jogging. You go in the black community, you see a few people walking or jogging. We don’t exercise as much. And I suspect that if you look at eating patterns, blacks will be consuming more carbohydrates and fats than whites. Whites generally are more health-conscious-the salads. In fact, I work with a lot of churches and talk about nutrition, and you get a lot of blacks at some banquet-put a bowl of applies and fruits and then you have all the fatty stuff around. You are going to see which is consumed the most.
RM: But that happens across the board.
SB: I think generally- I haven’t got the stats on this-blacks proportionally are getting fatter and fatter. More than whites.
RM: Could it be that-you said that white people tend to be more health-conscious for whatever reason. Maybe they are concerned with their own mortality more or something, but could it also have something to do with whites having more access to physicians, to educators, who tell them, you know, ‘If you keep eating ice cream every night before you go to bed, you might as well forget it?’
SB: That’s partly true, but I think there are many unexplored areas. I can’t explain why so many black folks are fat. I just can’t explain it-except the diet and exercise. Why with the variability of the collards and the mixed greens and the this and that we don’t see more consumption of that. Why do you find more tendency to exercise in the white community? I don’t know. You see, I can’t explain that. But those are the data, and what I’m trying to do-? that’s why I’m saying that my present job is one of the most enjoyable jobs I’ve had in a long time-I’m medical director of the Health Department.
RM: In Craven County?
SB: In Craven County.
RM: Oh, congratulations. I didn’t know that.
SB: Yeah, and what I’m trying to do is what I say initially a little cleverly-taking the Health Department to the people-giving the Health Department legs. Two or three nights every week, I go talk to churches and groups about two basic things–diet and exercise. Of course, I have to live this-not only talk about it, you know.
RM: You look like you’re doing a great job.
SB: You know, most people tell you that… I use this as my speech. What did I have for breakfast? And this is true. I’ve been eating this for breakfast for years-okra, broccoli, tuna, and whole? wheat bread.
RM: Oh my goodness.
SB: Now, the question comes-how come you can eat that? Well, something is wrong. Someone came up with this bacon and eggs stuff, and [these are] cultural things that we do. And I have to be responsible for my own health and my own dynamics. I’ve adopted it, and I sort of stick to it mostly, and I sort of repeat that during dinner. Lunchtime, I fall off the boat. You know, this is when I have access.
RM: Given to the cultural pressures during lunchtime.
SB: Yeah, with lunchtime. Of course, I’m partial to a honey bun every now and then.
RM: Well good. The balance is important.
SB: Yes, yes. So those are the things I’m trying to impress to people, and we are now actively working predominantly in the black community on chronic diseases-that is, hypertension? with those two strategies. In fact, we have a third one–diet, exercise, and decreased smoking. I’m looking forward to grants to help us…
RM: Wonderful.
SB: …get this over. What led up to that, because in the 1830 census, I told you that black slaves and freed men and women were living longer than whites. Maybe women equalled out, but the men did well also. But the white men didn’t do well. Now, it is reversed. One of my challenges is [that] I’m going to look at the census in the 19th century and the 201 century to see that change.
RM: Plot it.
SB: Plot it, yes. Because I don’t know what is behind this. I know the television had to do advertisements…
RM: I’m thinking the automobile had something to do with it.
SB: Something… Some dynamics are working out there. But something happened, and I think that blacks are the victims of what’s going on out there in the white world.
RM: Well, we’re all victims of many things that are going on as far as the way we take care of ourselves and our activities in the daytime. I’m sure that now that we’re removed from having to produce our own food, all of us do things that aren’t good for us. We sit still more than we ought to.
SB: Yeah, yeah.
RM: And eat what’s handy because we think we have to cram so much into a day that we eat whatever’s there, and it tends to be full of fat and sugar.
SB: Maybe I shouldn’t say this, but I’m going to say it anyway. The thought occurs to me that we as a culture feel that we need to go to the doctor more often than we need to. I say that because I think people need to be a little more independent-thinking, making decisions for themselves. After you have absorbed all this cultural intake of food and lack of exercise, then you got to go to the doctor ’cause you’re gonna get sick. But if you can control that, you’d have to go to the doctor less. You know, use a health-care facility. You need an annual checkup of course, but I know people–every six months, three months-‘I gotta go see the doctor, doctor, doctor.’ I think human beings have the ability to control their health much more than they’re accustomed to doing, and I think we need to think in terms of that. And it is very simple-no smoking. Get rid of tobacco altogether. I’m in eastern North Carolina; I have to say that. Exercise more and eat prudently-fruits and vegetables-and then you’ll see the doctor less. But it is very difficult to get this done.
RM: Well, it makes so much sense. Thank you for sharing all this wisdom with us.
SB: Yeah, but it’s a very typical thing to sell. Here’s a diabetic, 100 pounds overweight, stil1 is 100 pounds overweight, continues to eat-in spite of all the high-tech medical-in spite of you are going to keep doing this type of thing. How do you reverse the whole thing? I think preventive medicine should come up with some type of thought process.
RM: When I asked Dr. Best what he felt his most important contribution to healthcare had been, he said it was in education, and maybe that’s the key–early, early… teaching the children. So it’s ingrained-so it’s a part of…
SB: Yeah, and people somewhat like to be entertained. You go to educate some people-they’re proud, you know, ‘Very good, doctor-very nice’ (as he is clapping), and the next minute they’re going back to supersize it at McDonald’s. You know, so how do you change this? You gotta keep chipping away, chipping away, chipping away, and we need allies. We need allies in the churches. One of the things when I speak to churches, I refer to the Adventist Church that seems to have diet high in their agenda for salvation, and they really stress the diet; and I’m trying to get all the ministers to do that because there are many passages in the Bible that refer to dieting you see. And if I can get some allies in the churches, then perhaps…
RM: Oh, what a good idea.
SB: …you can get somewhere.
RM: People listen on Sundays. They do.
SB: Yeah, they do.
PC: Good morning. This is May 21, 2001. It is Monday, and I am in the presence of Dr. Sidney F. C. BarnwelL My name is Paul Cunningham, and we are at the Department of Surgery, East Carolina University. The purpose of this interview is to learn about the life and influences on Dr. Sidney Barnwell. This recording will be transcribed and kept at the Health Sciences Library at East Carolina University where it will be available as an oral history resource for people interested in the history of healthcare. Dr. Barnwell, do I have your permission to record our conversation?
SB: Yes, you do.
PC: Thank you. This conversation also begins where Dr. Ruth Moskop left off during an earlier conversation today. Dr. Barnwell, you spoke to Dr. Moskop about your early childhood and youth, and I was wondering if you would care to elaborate about perhaps any early influences in Guyana.
SB: I was born in 1926, and there were some things-dynamics-within the first 10 years. I remember one of the things that influenced my thinking about life as a whole very early on was when Mussolini went into Ethiopia, and there was created a lot of stir within the black community, and the other thing was Joe Louis in this country. You know, Joe Louis and Max Schmelling-that, again, engendered a whole lot of feelings-claiming superiority in this blackman-on Schmelling and so on and so forth. Early on also, American influences… I saw America only through the movies. You know, Duke Ellington, Count Basie, Frank Sinatra, and Bing Crosby-so that had a lot of influence on me. Prior to the Second World War, most people went to Europe to study, and my parents expected us boys-1had three brothers, I was one of four brothers-to go to Europe, but because of the influences and the Second World War, we all decided to come to the United States. In fact, I did; I left and came to the United States and went to Howard. Howard at that time was somewhat still a segregated university and the only university that people from Guyana went to. Some, perhaps, went to Lincoln University, but most went to Howard and studied medicine, dentistry, architecture, law, etc. I came to this country in 1947 and went to Howard-did undergraduate for three years, graduated, and went to medical school. I completed that in 1955. One of the interesting things-I finished college a little before time; instead of four years, I did it in three years and graduated with honors. Medical school was difficult to get in at that time because if you didn’t go to Meharry or to Howard University, chances of getting into other medical schools were very slim. Those veterans who were coming back from the Second World War had priority in medical school and dental school, so West Indians were given a small quota. We had to compete among ourselves. So after I finished undergraduate school, I lacked one course in Chemistry-qualitative analysis or quantitative-so they wouldn’t let me into medical school until I got through. So I went to Georgetown to the graduate school and spoke to the dean. The first thing I ran into: ‘You know, we at Georgetown don’t take blacks.’ He didn’t say it in so many words. So I stuck it out with Howard and got into medical school in 1951 and got through in 1955. Around 1950, my father died, and I experienced some adverse events in my life. There wasn’t any money coming from overseas, and literally I had to work my way through medical school. To conceive of that these days is very difficult. I had to take the 10:20 bus at night to get to the job at 11:00 until 7:00 in the morning. I would leave the job at 7:00 in the morning and get to school at 8. I did that for four years, and thank God, it was a switchboard job. I could study at the job, you know. But I did that six days a week and got through medical school. The school was very kind to me, and I graduated in 1955. Because of what Howard did, you know, Howard University was the center for black studies I think in this country-they called it the Harvard of Black Studies. There were many professors that prepared me for a life in Medicine, and they educated me well. I always feel indebted to those who made the sacrifice for me. I left Howard and did an internship at D.C. General Hospital. I wasn’t sure what I wanted. I did Dermatology Pathology for one year and then went back to Guyana, and Guyana then told me that they needed surgeons badly. There was Charlie Denbow’s father who was the kingpin. He was a Howard graduate-a dentist-and he got tons of people to Howard. Then I went back to Howard and Lasalle Lefoy was-I don’t know if he was chairman at that time-but he was very much-no he wasn’t chairman-he was still in training. The residency slots were full, so I went to Baltimore. There was a training session at Providence Hospital. You could do the first one or two years at Providence, and then you had to move on to another setting. I was there a couple of years and one year in Pathology at an accredited one-year program. The last three years I did in Philadelphia-’59 or ’60 to ’63 at the Mercy Douglas Hospital-another segregated hospital, and there were some good guys there who were board certified and did a good job of training surgeons. I got my boards in ’63-’64 and decided to go back to Guyana again, but there was civil unrest in Guyana-a mini civil war at that time-trying to get independence, and so me and my wife and a couple of kids decided to come back to the United States. I went back to Howard and went to the dean: ‘Hey, I’m here. I’m destitute.’ He assigned me to the VA Hospital in Tuskegee. That was a segregated institution because at that time most black veterans had to go to the Tuskegee VA Hospital. So I went there as a surgeon. They had a small training program there, too, for surgeons, so I participated in that. In 1965, I decided to come to New Bern because there was this black hospital-Good Shepherd Hospital-in New Bern that needed a doctor. That was a 60-something-bed hospital without a doctor. There was one doctor, Dr. Litman, who was there. He went to Tuskegee for training as a surgeon and was a resident, and he told me about the Good Shepherd Hospital, so I came there.
PC: Can you tell me, sir, what has happened to the Good Shepherd Hospital?
SB: Well, it’s now… It closed two years after I got there and is now a nursing home. There was an effort by the community at large to fund this hospital in the 1930s. As I told her, you know, there was a big fire in New Bern in 1922, and many blacks felt they were not treated fairly? those that were injured-and so they got together-a great community effort. It was spearheaded by the churches-one in particular, the Episcopal Church. In the 1930s, to build a hospital, it was about a 60-something-bed hospital, and as I told her, at one time (’65-’66), I had 33 patients in that hospital all by myself. That was hard work, and as a general surgeon I did everything-tonsils, hysterectomies, bones, general surgery-abdominal work. There was also the Craven County Hospital where I had privileges, but most of my work was done at Craven County Hospital. Patients were shipped back to the Good Shepherd Hospital where we gave postoperative care, etc.
PC: So could the patients stay in Craven County Hospital should you…?
SB: Well, yes and no. At that time-’65-the white surgeons who operated on blacks kept their patients there. When I went, in order to keep Good Shepherd open, we had to get the patients transported back to Good Shepherd Hospital.
PC: I see.
SB: Now that lasted for about two years, then integration came about ’68, and Good Shepherd closed, and I did all my work at the Craven County Hospital.
PC: Sir, I would just maybe like to take you back a little bit through all the early history. Are there any people influential in your life that stood out? Are there two or three names perhaps that really influenced your life early on and during the middle years up to when you moved to NewBern?
SB: I was blessed with outstanding parents. My father was well educated and had a big job in the railroad, so the resources were there. We were well educated-four brothers-well educated. I always point to the peer group of people in my early teens. We felt that… The war was going on, and we had a bonding, and the people I associated with felt that education was the answer to whatever the future held, so we supported one another. I could think of dozens of guys and young ladies who went on to achieve lots of good things in the world. So, that support was there through high school and the Cambridge exams, etc. I remember when I was 15 I was somewhat nonplus. I didn’t know exactly what I wanted to do, and I remember one day a young man who was about four or five years older-he had a way with the ladies-and so I sort of looked up to him. He said, ‘Sidney, you’re gonna be a doctor.’ You know, I just looked at the guy. I’ll never forget that, you know, and that really influenced me. He sort of put me in the right direction. And there were influences, Claude Dimble, and the older generation who felt that we all need to be thinking in terms of independence of Guyana, leadership of the country, education, etc. So those are the things that really led to my career at Howard and, as I mentioned before, getting into surgery-influenced going back to Guyana-coming back to the United States to study surgery. When I mentioned some things to do with the Health Department where blacks were concerned, where there was a disparity in healthcare, I felt that I had to fill that gap, so I stuck with the Health Department through prenatal care, maternity care, and eventually family planning issues. The politics-1 lived through the civil rights time-and that did not influence very much how I practiced Medicine. Black patients came to me primarily in ’65 because they had no place else to go. It seems as though, as integration came in the 1970s, those who got the opportunity to get educated seemed to want to go to white doctors. That was sometimes the trend of the day. From ’65 to about ’72, I did a lot of surgery, and my minimum surgery was for me to do three majors and three minors per week, and I felt very comfortable doing that. If I got over that, it got overwhelming, and so three majors/three minors-I could increase the minors but not the majors per week. When I went to New Bern, I was board certified. That gave me entry into the Surgical Department there. There were three white surgeons who were board certified. There were other surgeons-maybe one or two–who were not. I remember two events: The first month, one of the ladies-still in New Bern-she had a horrendous car accident. [She was] sitting in the front seat, crashed into the windshield, and mangled her face, and I saw her in the emergency room. Because I did a little plastic surgery in my training, I took some time, used the right sutures, and the nurses were so impressed. I mean, that was the talk after the whole thing was that the lady looked as though she had had the greatest surgeon in the world that fixed her up, and she healed well. Boy, that really elevated me-for nurses and people who dealt with the ambulance-they were talking-‘This new black doctor did this thing. And everything I brought-vagotomy-as a new entity to the hospital-lots of surgeons used to look over my shoulder, you know-to see how this is done, and that got me into the Surgery Department. Then, of course, the politics… You had to participate in committees and do the things for a hospital. So that really helped me for the first 10 years or so. As I told her, after the first 15 years, more surgeons came to the medical school, and there was competition between Craven County Hospital and this medical school I was affiliated with this medical school and, not surprisingly, Craven County didn’t like that very much, and so some unpleasant things happened. I remember in 1984 I really got mad with one doctor, and I had to take him in a room, close the door, and man, I cussed this bastard out because, I mean, it was obviously just inferior things, you know. And I began to see things which the average black surgeon would-who was born in this country-would run against, you know? And I had to address it accordingly. So, those were the days when the general surgeon did everything in New Bern. I had training in Orthopedics. I had trained to do Plastic Surgery. I did very little vascular work-very little when I went-but Dr. Charlie Ashford, who was trained at Johns Hopkins and came with his chest boards in about 1969-1970, he and I teamed up. So I was able to help him and he helped me. I used to do hysterectomies, also. So we had a close bond, and that bonding was very helpful in all of the competitive things that were happening with the other surgical group. The other surgical group got larger and did more specialized work, so Ashford came with chest boards and lots of other guys came in with Orthopedics? more GYN people came in. We had a neurosurgeon that came in, and so instead of sending patients to Duke or Chapel Hill, most neurosurgery was done in Craven County. We had some good X-ray people and some good X-ray conferences. I felt that even though it wasn’t felt over here, most doctors over there felt that Craven County Hospital was as good as anything that Greenville could come up with. I wanted to keep it so. But predominantly, Duke and Chapel Hill were the stars. ECU had to prove itself.
PC: So obviously, there was some initial tension and trepidation.
SB: Yes.
PC: How did that evolve to this point? How do you think it has gone through the years to this point?
SB: Well, you know, I went to New Bern in ’65 and left in ’85 and went to Tennessee, and I came back in 1998. Open heart surgery was established in New Bern, and I think, with the help of ECU, they had to prove themselves-so many cases per year, etc.-and again, the competition, in order to keep your caseload up, you had to make sure that you attracted patients. I have a feeling it is still there-the competition, the numbers. If nothing else, survival of the hospital. I am on the hospital board, and right now it’s called the Craven Regional Medical Center. Things are not hospitals anymore, they’re medical centers. In order to survive, of course, you have to have patients. We have good leadership, and we are doing fairly well while many hospitals around us-Jacksonville, in particular-are doing poorly. So, we point with pride? Pitt is doing well, but we are also doing well.
PC: It seems, then, that the old dynamics-Duke and Chapel Hill-were the primary… They were way up there, and Pitt Memorial and East Carolina University had to yet prove or sell itself? IS years ago. Has that changed?
SB: I haven’t been able to ferret out that because I was always interested in that. Right now, I am at the Health Department. I don’t practice Medicine. I think things have softened a little bit. Referrals are made, but again survival… The difficult cases are most probably sent here, but for survival you want to be able to keep your patients, and so that competitive edge is still there.
PC: All right, sir, I’m going to change gears a little bit and just ask you a couple of questions about yourself. Are there are any specific skills that you feel were most important to your success in life?
SB: A relationship with people. I think no matter how well you are skilled, if you cannot get along with your peers, if you are not capable of resolving small things before they get to large things, if you cannot capitalize on the assets that are around you, it’s to your detriment. You have to be able to get along with people. You have to be able to build a consensus. You have to, as the politicians would say, have people vote for you. In order for that to happen, you have to demonstrate the ability to hold on to those who have placed their trust in you. That means you have to prepare yourself-be a very competent person. Since my residency days, I get up early in the morning-at 4:00—to study. I don’t practice anymore, but I still do that because it’s just part of my degree of thinking. I left here in 1985 and went to Nashville, Tennessee, to the General Hospital. Meharry Medical College just began working as a general hospital [and] was dominated by Vanderbilt. I had to prove myself to Vanderbilt, and what took me through was two basic things: I can out-study anybody-I always said that-and so I was able to get the academics together. But secondly, I had to get along with people who Meharry felt were racist, and I had to overcome that. My counterpart from Vanderbilt, a very delightful–one of the most skillful surgeons I have seen? may see this, and I may have to take a wheelbarrow and pick him up. He had a full professorship in Anatomy and Surgery and, you know, would have charts. Two or three months after I got to the General Hospital, he gave a grand rounds at Meharry, and his first statement, he said, ‘One of the best things Meharry has done is to get Dr. Sidney Barnwell to the General Hospital,’ so we were able to bond. The ability to do that is very important.
PC: You clearly have been one, then, who is not afraid of learning new information. Are there any new skills that you feel that every human being in our profession-of Surgery-needs to learn in order to remain effective?
SB: How to get along with people.
PC: Absolutely.
SB: I mean, that is so basic. Regardless of how skillful you are as a surgeon, you are going to be an SOB and nobody wants to be around you-the nurses or nobody-you know, and I think it’s just lost. The other thing I think we need to do is to get away from the academia and look at the world at large. Right now, a quick assessment I made of New Bern still holds. When I look at the black population: Education-poor; economics-poor; health/disparities-poor; the environment-poor. There are more blacks in jails. And I learned this figure: 5% of the world’s population are in the United States-just 5%, or a little less than 5%. Twenty-five percent of the people in jail in the whole world are in the United States, and over 50% of those are black. I mean, those are issues out there-they are there. Regarding the merits, they’re there. So, the poor health, economics, environment-they’re there, and I think we educated people need to look at that away from our chosen profession. How can we in small ways address those big problems? In my new career as medical director of the Health Department, I’m trying to do just that. I can’t cure world hunger, but I can select out health. I’m looking at chronic diseases within the black community and what I can do to address those things.
PC: Well, if you were going to speak to surgeons, they might tell you that that’s not their concern. They are surgeons and they go the operating room. Do you agree with that, and how would you advise surgeons today?
SB: Surgeons first are human beings, and there are human problems out there. You don’t have to devote 100% of your time, but you have to live in a world where these problems are. [In the instance of] world war or any type of disaster, we somehow find the time to help other people, and we have to look at the world around us to see what we can do in some way-in kind or in cash or make some contribution towards that. I have more time to do that right now, and I’m addressing that from the preventive point of view. But we need to look at other issues because they are going to overwhelm us.
PC: Has the relationship in your mind changed between physicians and surgeons over the last 20 years, and how would you characterize that?-if so.
SB: I think managed care has a lot to do with it these days. Surgeons used to be prima donnas. When I was in training, my goodness, I have told about a famous chairman of a department. He was in such high regard, and the residents used to walk a couple of paces behind him-this is true. He was a stickler for cleanliness, and one day he looked and saw a cigarette butt just in front of the elevator. So he stopped and looked at the cigarette butt, and the chief resident looked at him, and then he looked at his chief resident who quickly picked up the cigarette butt and discarded it. Anyway, that has changed. They are more collegial at this point, and managed care has forced a lot of different dynamics-where the family practitioner now is held in some high esteem.
PC: Sure. How do you discuss the perfect career if you are going to advise somebody as to developing the perfect career? Do you have any thoughts about that?
SB: You are going to my spiritual dynamics now. I think each person in this world has a propensity for certain occupations. I just saw my plumber-he’s one of those guys. If you know what that is, you should embrace it very early on. The problem is-in the world in which we live-we are programmed in grade school and high school-you have to do the basic coursework….in order to amass that expertise in various subjects. But if in your college career with all the liberal arts you can discern the perspicacity to pick that out-which appeals to you-regardless of whether it’s one that would make you a doctor or an Indian chief. If you seem to love art, if you seem to love music, you stick with it. You are going to make a great contribution because that is the thing that is going to drive you to put in the extra effort in order to maximize that which is potential in that specialty or in that work occupation.
PC: Thank you. Now, looking back on your life, is there any particular lesson of leadership that students should draw from your experiences and would be useful to them in their role as leaders of their communities? Any additional thoughts about that? You already shared with us that you need to respect others, but…
SB: Well, a physician/doctor in most communities is still held in high regard. I think the character question is something which should be paid a lot of attention to because people put their trust in you as a physician, and you need to live up to that. And I think as a role model, you can act as mentor to those who are less fortunate just by being who you are is one thing, and then if you have the time, actively do something within that community to help to build that community up.
PC: As far as the future is concerned, how can the medical community deal with the pressures that are out there and still maintain its traditional identity?
SB: I forgot the name of that organization-Doctors Without Borders-is that close?
PC: That’s close.
SB: That’s close enough. We need to do more of that. Doctors sometimes are perceived as money hungry. You can look too much at the business of Medicine, and I think many young people are in debt when they are in medical school-that’s understandable-when you have to pay back your debts, but on the other hand, there are many young people who want to get into a Mercedes early on and forget that the basic idea of getting into Medicine is for compassion, wanting to help people, wanting to make a contribution. I think we need to emphasize that more in medical schools.
PC: How do you think Medicine and Surgery, in particular, are going to look 25 years from now if you can look that far into the future?
SB: Sometimes I’m very optimistic and sometimes pessimistic. The pessimistic part of it-if we continue to be that mercenary as I see some young doctors are-1 think we are going to just be considered business people. From the optimistic point of view, there is still an opportunity, a window, to expand the care and compassion part of Medicine that’s been traditional for centuries. If we can explore that then I think we’re going to be pretty well off in 20 years.
PC: Sure. How do you grade yourself as having accomplished what you set out as your own career goals over these many, many years?
SB: Well, I grade myself A+. I got the right wife. I tell you, I got the greatest mate, and I was lucky. That really helped my career. There are many areas that on the face of it, when I looked at it on the face of it, I felt that I was not making the right move; but on reflection 10 years after the fact, I was able to appreciate the right move. My accountant told me in 1983-’84-’85, ‘You are spending too much time in the community. You gotta practice a little more.’ And I said, ‘Maybe you’re right.’ But in reflection, that was the right move because what happened when I left New Bern and went to Tennessee and worked at Meharry and then spent eight years at the VA Hospital and decided to retire, I made one telephone call to the folks in New Bern. ‘I’m coming back to New Bern.’ And the next thing is, ‘We want you as our medical director of the Health Department.’ You see, I’d laid the groundwork years ago with the Health Department, and again, you know, there are pains and then you grade yourself. At what point in life? But throughout my life, since I got married in 1955, my greatest asset has been my wife.
PC: That’s a wonderful thing. Do you have any regrets concerning some of the goals that you set for yourself early on and might not have attained through your years of service?
SB: Yeah, one main regret, and my wife says, ‘You should be happy,’-1 didn’t go back to Guyana to practice Surgery. But on reflection, that was the best thing I’ve ever done because Guyana has gone downhill. They adopted a communist model, and it took 20 years to crash, and many guys who went back there had to leave with their suitcases. I mean, Guyana’s currency was zilch. Many of my friends came back to the United States after giving 15-20 years to Guyana. I never had that opportunity. So my wife is happy of that. I regretted it at the time; on reflection, it was one of the best things that happened to me.
PC: What do you feel that people will think of you in the year 2050?
SB: That’s a difficult question. I have to reflect on those who went before me, say 30 or 60 years ago. Many doctors who were in New Bern-nobody even heard about them. I am sure they made great contributions in generations past. Unless you record it, nobody knows you were there-just like a tree falling in the forest. What they will say is what we record. I’m happy one of the things-most happy things-that’s for your equal. When I went to Tennessee, nobody knew me. I didn’t practice really as I practiced, and I spent 13 years [there]. I came back in 1998, and everywhere you go in Craven County, ‘Hi, Dr. Barnwell. Glad to have you back.’ It does a lot for your ego, you know? People are glad to have you within their community, and what people would say I don’t really know. I don’t rea1ly know. My ego would tell me, ‘I hope they say kind things.’
PC: Do you have any final comments that you’d like to mention in the last few minutes of our discussion this morning?
SB: I am very grateful to this medical school-Dr. Beekman, who gave me an opportunity to become Associate Professor of Pathology-Or. Laupus, who was Dean and I became assistant dean-and Dr. (your chief surgeon, what’s his name?)
PC: Dr. Pories.
SB: Dr. Pories invited me up here, and I came to conferences. So that association I hold very dearly, and that contributed very much to my staying in New Bern over the years.
PC: Again, I’d like to thank Dr. Barnwell for taking time this morning to come and talk about his experiences in eastern North Carolina. We would like to say that we hope that this will not be the last time that we’ll have an opportunity to talk and discuss the exciting life that you have had in eastern North Carolina. Thank you very much.
SB: Thank you.
Citation:
Barnwell, Sydney. Oral History Interview with Dr. Sydney Fitz C. Barnwell. 21 May. 2001. Oral History Collection. LL02.03.02.03. East Carolina University Digital Collections. https://digital.lib.ecu.edu/57053 and part of this collection https://digital.lib.ecu.edu/special/ead/findingaids/ll02-03.
Credit, courtesy of: The William E. Laupus Health Sciences Library, East Carolina University, Greenville, NC.